<iframe style="width:120px;height:240px;" marginwidth="0" marginheight="0" scrolling="no" frameborder="0" src="//ws-na.amazon-adsystem.com/widgets/q?ServiceVersion=20070822&OneJS=1&Operation=GetAdHtml&MarketPlace=US&source=ss&ref=as_ss_li_til&ad_type=product_link&tracking_id=peaceinvesting-20&language=en_US&marketplace=amazon®ion=US&placement=0060555661&asins=0060555661&linkId=80f8e3b229e4b6fdde8abb238ddd5f6e&show_border=true&link_opens_in_new_window=true"></iframe>|<iframe style="width:120px;height:240px;" marginwidth="0" marginheight="0" scrolling="no" frameborder="0" src="//ws-na.amazon-adsystem.com/widgets/q?ServiceVersion=20070822&OneJS=1&Operation=GetAdHtml&MarketPlace=US&source=ss&ref=as_ss_li_til&ad_type=product_link&tracking_id=peaceinvesting-20&language=en_US&marketplace=amazon®ion=US&placement=1119404509&asins=1119404509&linkId=0beba130446bb217ea2d9cfdcf3b846b&show_border=true&link_opens_in_new_window=true"></iframe>|<iframe style="width:120px;height:240px;" marginwidth="0" marginheight="0" scrolling="no" frameborder="0" src="//ws-na.amazon-adsystem.com/widgets/q?ServiceVersion=20070822&OneJS=1&Operation=GetAdHtml&MarketPlace=US&source=ss&ref=as_ss_li_til&ad_type=product_link&tracking_id=peaceinvesting-20&language=en_US&marketplace=amazon®ion=US&placement=1119376629&asins=1119376629&linkId=2f1e6ff64e783437104d091faaedfec7&show_border=true&link_opens_in_new_window=true"></iframe>

By Dr. James M. Dahle, WCI Founder
The House of Medicine is a surprisingly stable place. Over the years, the highest-paying specialties—like neurosurgery, plastics, and orthopedics—have been among the most difficult to match into, and the lowest-paying specialties—like PM&R, preventive medicine, pediatrics, family medicine, and internal medicine—have been among the easiest to match into. Other specialties are somewhere in between. For my entire career in emergency medicine, we have been in between. We've been about midway up as far as pay goes and as far as competitiveness in the match.

Typically, about 93% of US MD graduates who want to match into EM are able to do so. Usually, there are very few spots open for the SOAP (scramble). Seriously. Like a handful. And it was a huge embarrassment if your program had one. So, imagine the shock and awe that hit emergency medicine during Match Week 2023 when it was revealed that the number of unmatched positions had increased by more than 100X. That's right, 555 residency spots were entered into the SOAP in March 2023. That's out of just 3,011 total spots, meaning 18.4% of spots went unmatched. Compare that to internal medicine (545/11,911 = 4.6%) or family medicine (589/5,100 = 11.5%).
Emergency medicine has officially become the easiest specialty to match into. It is now the least competitive and arguably the least desirable to medical students. What happened, and can it happen to other specialties? Is there something unique here, or is EM just the canary in the gold mine as the ED often is for our broken healthcare system?
What Happened to Emergency Medicine?
This is likely multi-factorial, and there may be dozens or more factors that have contributed. However, I think there are four main reasons, and I'm going to list them in the order in which I think they contributed, starting with the most important.
#1 Too Many New Residency Positions
Not many years ago, it was determined that we were not going to have anywhere near as many emergency physicians as we needed, especially if we wanted to staff rural EDs with emergency physicians instead of the internists, family practitioners, general practitioners, and APCs that have been working in them. There was encouragement to start more residencies and to expand the existing ones. Contract management groups and for-profit hospitals started having trouble staffing their EDs and found themselves having to pay $400 or even $500 an hour to staff undesirable shifts. They decided to do something about it. They started their own residency programs. Somehow, despite having few experienced academic faculty members or any sort of track record, these residencies were approved and opened. The number of training slots in EM has ballooned over the last few years. Mary R. C. Haas, et al, published an article in 2020 titled “Too Big Too Fast: Potential Implications of the Rapid Increase in Emergency Medicine Residency Positions.” The paper included this chart:
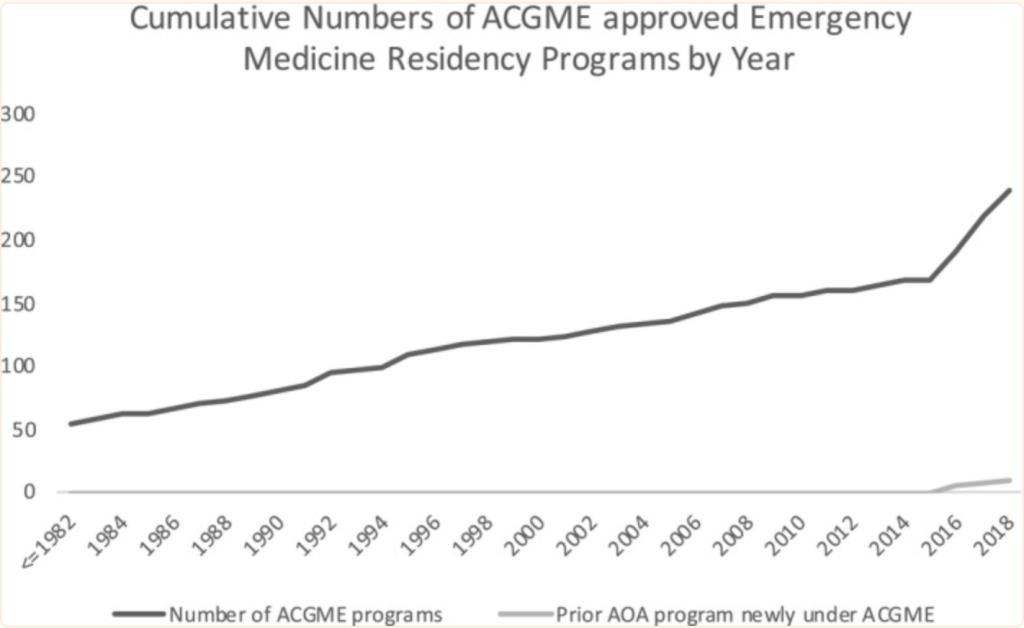
Check out the change in slope after 2015. The increase in the number of training slots has been even more impressive.
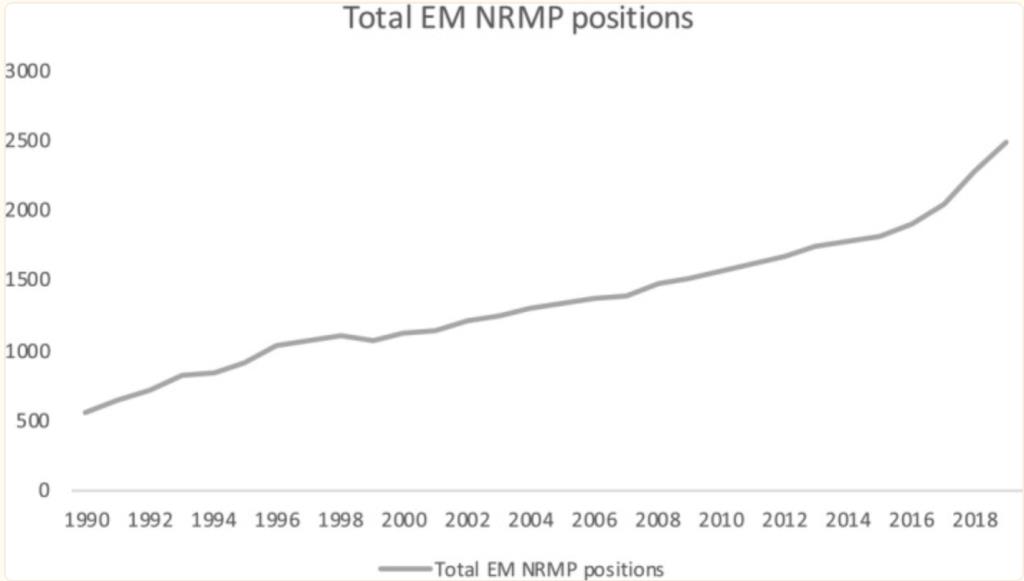
Remember this chart ends in 2020. The 2023 number is 3,011. In three decades, we've 6Xed the number of residency spots. We've more than doubled the number of spots since I graduated in 2006. The number of spots since 2015 has increased by 65%. That was the year that this year's EM residency graduates were applying to medical school. Sixty-five percent. That's a massive increase. Yes, the entire Match has gotten bigger in that time period. PGY1 positions for all specialties increased from 27,293 to 36,277 (a 33% increase). But the increase in EM was double that.
The paper speculated about the implications of this increase. The authors' worries included:
- New graduates unable to get a job
- Zero-hours contracts where new hires are not guaranteed any hours
- Worsening primary care shortage (due to more people going into EM rather than primary care)
- Increased difficulty paying off student loans
These new EM programs are clearly a concern for these students considering entering the field of EM. One needs only to peruse online forums such as the r/emergencymedicine subreddit or the EM subforum at StudentDoctor.net to find out what current and potential residents think of the new programs, particularly those started by hospital corporation HCA. Consider this post: “SOAP warning EM HCA residency” where a PGY3 created a throwaway account just to bash their own residency.
As this person wrote:
“Please let this be a warning to all medical students planning to SOAP into a HCA residency. I am a PGY-3 EM resident at a HCA EM program. My experience at this program has been the absolute worst and one of the biggest mistakes I have ever made. I have suffered through for 3 years because I had no other options after $400k+ student loans and a family to support.
Speaking with friends at other HCA programs, a few things are recurring themes, including continuously adding on scut work and shifts for residents to milk every dollar they can, having no organization or constant leadership for programs, constantly having ‘away rotations' to try to meet bare minimums for procedures (many of my colleagues have not completed all required procedures including lumbar punctures, deliveries, trauma resuscitations, etc.) We have constantly rotating ‘faculty,' many of whom have no interest in residents or teaching and are just here for a quick locums gig. I honestly feel totally unprepared to even begin practicing on my own.
We are constantly getting new requirements to meet certain metrics from the HCA overlords and pressure on shift from malignant attendings to meet them. There is hardly ever any organized didactics, and forget about teaching on shift; you will be just trying to meet the endless metrics and keep the patients moving. It it clear that all HCA wants to do is exploit cheap labor and increase their bottom line, and your training as an emergency medicine resident is not a priority. To top it all off, many of us are still struggling to find jobs. Sure, there are some openings in rural wherever but none of us have signed in a desirable location and over half of us are still looking for a job. We have no support or connections to help us through the job process.”
These facts/opinions are clearly out there among MS4s based on the results of the initial pre-SOAP match. These figures are the list of unfilled spots/total spots for the HCA sponsored programs:
- HCA Healthcare East FL Division GME: Emergency Medicine/Aventura 8/12
- HCA Healthcare East FL Division GME: Emergency Medicine/St Lucie 4/5
- HCA Healthcare East FL Division GME: Emergency Medicine/Westside 8/13
- HCA Healthcare/USF Morsani GME-Brandon-FL 8/12
- HCA Healthcare/USF Morsani GME-Oak Hill-FL 5/6
- HCA Houston Healthcare/U Houston-TX 6/13
- HCA Medical City Healthcare-TX 1/8
Forty out of 69 spots (58%) at these HCA residencies didn't fill. How would you like to be the lone doctor in either of those two residencies where you're the only doctor who actually wanted to go there?
Last year, there were more than 200 unmatched spots. This year, there were over 500. Clearly, the article in 2020 was right. EM has gotten too big, too fast.
#2 Jobs Forecast
EM really did this to itself. Besides the Residency Review Committee (RRC-EM) approving all of these new residencies (and possibly having way too low of standards for approval), we published numerous “The Sky is Falling” type articles about there being no future jobs in EM. Despite not having a functional crystal ball, our most prominent journal in 2021 published a projection of EM workforce supply and demand for 2030. Here are the results of its study, and the conclusion from the abstract:
Results
The task force consensus was that the most likely future scenario is described by: 2% annual graduate medical education growth, 3% annual emergency physician attrition, 20% encounters seen by a nurse practitioner or physician assistant, and 11% increase in emergency department visits relative to 2018. This scenario would result in a surplus of 7,845 emergency physicians in 2030.
Conclusion
The specialty of emergency medicine is facing the likely oversupply of emergency physicians in 2030. The factors leading to this include the increasing supply of and changing demand for emergency physicians. An organized, collective approach to a balanced workforce by the specialty of emergency medicine is imperative.
If you were an impressionable MS3 and you saw that, would that make you more or less likely to go into EM? All of those folks that were on the fence about it probably decided to apply to another specialty.
Medical students have been concerned about Advanced Practice Clinicians (APCs: i.e. NPs and PAs) taking all of their jobs since the first PA graduate showed up on the scene in 1967. This was certainly a concern when I was a pre-med in the 1990s. It seems worse now that there are so many online NP programs and plenty of states that allow independent NP practice. There is even at least one ED in the country that is run entirely by APCs, despite at least one EM-specific paper showing APCs provide no economies of scale and another showing worse outcomes and higher costs. However, even in the workforce projection, only 20% of ED patients will be seen by APCs in 2030. I can't imagine that number is any lower in primary care or even in specialty clinics. I think this fear is probably at least somewhat overblown among students, although there is data showing more ED patients are being seen by APCs (an 18%-25% increase from 2010-2017) despite rising acuity.

#3 The Pandemic
The pandemic wasn't easy on any of us, but it was particularly tough on EM. My residency mate was the first doc to get COVID when it hit the Seattle area. He barely survived after weeks on ECMO. First, our volumes (and pay) dropped 40%, and many almost went broke. Then, when the pandemic finally made it from Seattle and New York City to our towns, our volumes surged and our staffing collapsed. Everything is slower and harder when you have to do it in full PPE. ED boarding increased. We ran out of PPE. It took me literally years to feel comfortable throwing away those precious first few N95s I could get my hands on.
I still remember those first few shifts. It felt an awful lot like being deployed with the military and not being 100% sure you were going to come home to your family. Worse, it felt like you were bringing Al Qaeda home with you at the end of the deployment. It was hard. It's still hard. As I write this, my hospital still (more than three years later) requires me to wear a mask the whole shift, and I can't admit any psychiatric patients without a COVID test. Burnout went through the roof. EM was always a high burnout rate specialty. It's worse now.
#4 Job Got Worse
EM, as a job, has been worsening over most of my career. Hospitals change corporations and EMRs every few years. EMTALA, HIPAA, board certification hassles, specific mandatory CME (stroke, trauma, opiates), and merit badge medicine (ATLS, ACLS, PALS, etc.) all contribute. A bigger issue is the increasing corporatization of medicine. Only about 8% of emergency doctors own their jobs, and even those democratic groups may have the worst business in America. Between 20%-40% of patients are self-pay (aka no-pay), and in reality, you only have one client—the hospital. If the hospital drops your contract, your business folds. When they say, “Jump!” we say “How high?” I don't know any partner docs that would prefer to be employees.
Recent laws against “surprise billing” (better titled “surprise coverage gaps”) have put downward pressure on emergency physician incomes. While nobody likes a surprise bill, emergency physicians have no recourse against insurance companies that refuse to contract fairly with them. This isn't only theoretical. After these laws were passed, Blue Cross Blue Shield of North Carolina proposed in-network contract termination for physician groups unless they agreed to 15% payment reductions, and United Healthcare proposed the termination of physician contracts unless they accepted a 40% paycut. Hospital systems are more and more likely to be owned by corporations and private equity with a relentless focus on metrics and profitability. Even when they try to focus on improving the patient experience and quality of care, they end up measuring the wrong things and do so in non-statistically significant ways. It's just not as good of a job as it used to be.
More information here:
What Happens If You Don’t Match Into Residency and What to Do
Consequences
Now that EM is no longer a competitive specialty to match into, what is going to happen? Let's start with what is not going to happen. Those programs aren't going to not fill. Those spots will just be filled in the SOAP. More than 95% of unmatched positions are filled in the SOAP these days. It's the doctors who are left holding the bag, not the programs. Between 6%-8% of US MD and DO grads (and as many as 50% of IMGs/FMGs (15% overall)) don't match anywhere. For many IMGs, any residency is better than no residency. The overall SOAP has become much more competitive in recent years as the increase in residency spots has not kept pace with the increase in medical school graduates. Believe it or not, there were times in the 1970s and '80s when there were more residency spots than applicants in the match. There will be more DOs, IMGs, and FMGs in EM programs that have not traditionally taken DOs, IMGs, and FMGs.
There won't be less pressure on the EM job market either. Since those programs are going to fill and graduate residents, it's still going to be nearly impossible to get jobs in highly desirable places and increasingly hard to get them in less desirable places. While I have no idea how accurate the EM workforce projections for 2030 really will turn out to be, there's no reason to think the decreasing competitiveness of EM in the match is going to change that.
Emergency physicians won't be paid more either. The supply and demand calculations haven't changed. Besides, medicine isn't really a functional market anyway. Supply and demand have little to do with how much most doctors are paid.
What is going to happen is that EM residencies are, on average, going to be filled with less competitive applicants. Instead of filling with people in the top half of their MD med school class like most of the residencies I applied to 20 years ago, they'll have a combination of top MD applicants, less competitive MD applicants, DOs, IMGs, and FMGs. That will likely make the job of residency faculty more difficult than it has been in the past, especially those faculty in brand-new, corporate-sponsored residency programs that may not even want to be faculty anyway. Over time, the quality of the physicians in the ED is likely to decrease at least somewhat. While one specialty's loss will presumably be another specialty's gain, it does make me sad.
More information here:
My Spouse Is Quitting Medicine
Are Physicians Who Retire Early Abusing the System That Made Them Rich?
What Is to Be Done?
The major organizations in EM put out a joint statement, and they are creating a task force. Most are skeptical that it will really do anything. Our biggest organization, the American College of Emergency Physicians (ACEP), is widely viewed in the specialty to be “in bed” with corporate medicine—particularly the large Contract Management Groups (CMGs)—and many feel they have a massive conflict of interest in matters like these (57% of revenue for the organization is not from dues). However, there are a few things that can and should be done. They cannot all be done by emergency physicians themselves, unfortunately.
#1 Quit Approving Crappy Residencies and Put the Current Crappy Ones on Probation
The RRC-EM needs to be strict, especially if we're dealing with less qualified docs entering programs. If residents aren't getting the clinical experience, procedures, and didactics they need to be great docs, their residency programs need to be fixed or shut down. Yes, it stinks to be a resident in a program on probation or in one that closes. But hiding the problem doesn't make it go away.
#2 Make Fair Surprise Coverage Gap Laws
More work can be done here to ensure that insurance companies don't take advantage of hospitals and physicians, particularly those forced to work for free due to EMTALA. While we're at it, how about funding EMTALA? Also on my Christmas list is adequate funding of Medicare and especially Medicaid. We're not supposed to lose money on “insured” patients. EM is always going to be a tough job. It should be paid like it.
#3 More Physician Ownership
We need to do everything we can to boost physician ownership so they can control their own jobs. Doctors need to be the ones deciding how to deliver care, how to staff their own schedule, how to split up the earnings of the business, and who they work with. The corporatization of medicine is bad for doctors and patients. Our organizations need to support physician-owned models and hospitals, and patients and government entities need to be educated on the benefits of long-term, stable doctor-owned businesses providing their care.
#4 Better Community, Government, and Hospital Support of Emergency Departments
In some ways, emergency departments are like fire departments, police departments, and public health departments. There needs to be some slack in the system so when the excrement hits the ventilatory system, there is room to flex. There should be some people standing around in the ED not doing much most of the time so that when it gets really bad, there are enough resources to take care of a rapid influx of patients. If the hospital cannot afford that, the community and government entities need to make up the difference. Frankly, just funding EMTALA would probably be enough.
I can't make my grocer, landlord, or pharmacist work for free, but somehow I can make my emergency physician (and on-call colleagues) do so? That's not right. Ensuring doctors and hospitals got paid something for the no-pay patients would go a long way to providing slack in the system. Perhaps we need a great compromise: hospitals and doctors promise to overstaff and society agrees to pay for it. Frankly, EM probably isn't the only field that needs this. Have you tried to place a patient into a pediatric psychiatric unit lately?
#5 Quit Complaining to Students
I like to whine as much as the next doctor. Doctors are pros at it. In the military, there is a saying that “Complaints go up.” That is, you only complain to your superior officers, i.e. the people that can presumably do something about it. If we want the best students to join us in emergency medicine, we have to quit “complaining down” about the current situation to impressionable pre-meds and medical students. I don't mean that we should hide the truth from students. Emergency medicine has always had its warts. But let's make sure they also hear about all of the best parts.
Emergency medicine is a great specialty. The medicine and the patients are interesting. Everyone has an ER story, for better or worse—you get to make a difference on the worst day of people's lives. You can still be the white knight of medicine. But it has issues, and if they are not resolved soon, the House of Medicine is going to regard us exactly the way it did when we started the specialty: losers, castoffs, leftovers, and chumps.
What do you think? Why do you think this happened and what should be done about it? What lessons should other specialties learn from this? Comment below!
The post Emergency Medicine’s Popularity Plummets appeared first on The White Coat Investor - Investing & Personal Finance for Doctors.
||
----------------------------
By: The White Coat Investor
Title: Emergency Medicine’s Popularity Plummets
Sourced From: www.whitecoatinvestor.com/emergency-medicine-popularity-plummets/
Published Date: Wed, 22 Mar 2023 06:30:09 +0000
Read More
Did you miss our previous article...
https://peaceofmindinvesting.com/investing/how-to-make-more-money-than-your-friends
.png) InvestingStocksToolsClubsVideosPrivacy PolicyTerms And Conditions
InvestingStocksToolsClubsVideosPrivacy PolicyTerms And Conditions
